Isolation is not the answer
There is hope, even when your brain tells you there isn’t.
— John Green
Is anxiety everlasting? Is this an intrusive thought or a hallucination? One of the most difficult things about mental illness is questioning yourself and reality, but it’s important to untangle your feelings and be confident to ask questions – even if the answers aren’t always there.
What exactly is a mental illness?
According to the National Alliance on Mental Illness (NAMI), a mental illness is a condition of the brain that results in disturbances of a person’s thinking, feelings, mood, or behavior.
There are many different types of mental disorders, and they each have unique presentations. Among them, they can are typically characterized by abnormal thoughts, perceptions, behaviors. These disorders can be lifelong or short term, and can have a variety of overlapping causes, such as genetics, the environment, or lifestyle behaviors. They have the ability to impede on day-to-day functioning, and can make it difficult to handle the ordinary demands of life. Currently, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is used to classify mental disorders based on diagnostic criteria unveiled through research by experts in the field.
How common are mental illnesses?
- About 1 in 5 people in the United States experience mental illness.
- About 1 in 25 experience serious mental illness, such as schizophrenia, bipolar disorder, or major depression.
- Nearly 1 in 7 children and adolescents are affected by mental health disorders.
- Anxiety disorders, such as post-traumatic stress disorder (PTSD), generalized anxiety disorder, obsessive-compulsive disorder (OCD), have the highest prevalence, affecting 19.1% of U.S. adults aged 18 and older
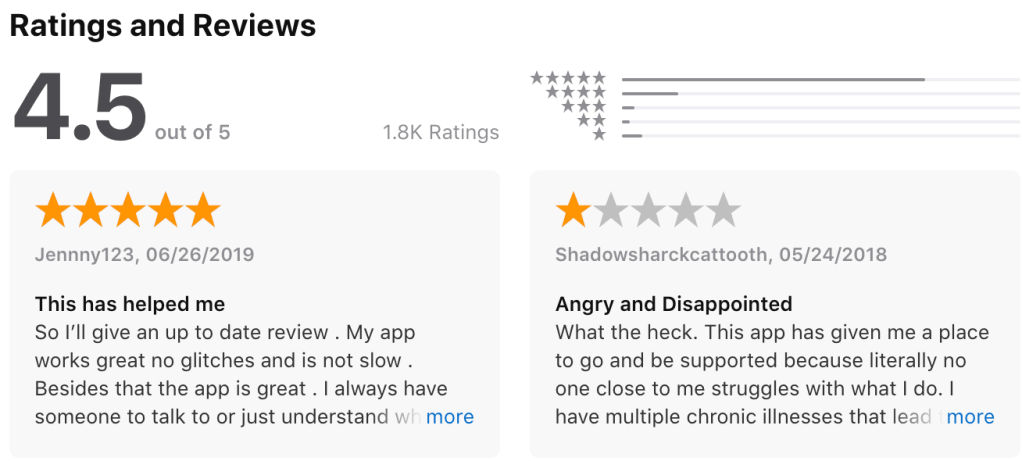
Yet, less than half (43%) of adults with a mental illness receive treatment in a given year. Why?
Research has shown that individuals with mental illnesses tend to generally possess negative attitudes towards seeking help, the cost of treatment, feeling like they can handle the “problem” on their
own, or even carrying the belief that the treatment will not help.
But, there is growing evidence to show that barriers to seeking help and recovery for mental health problems include the public and perceived stigma around mental illness. Stigma can perpetuate harmful attitudes and stereotypes about what it’s like to live with a mental health condition, and can ultimately dissuade individuals from seeking help.
Moreover, stigma has been linked to lead to misunderstandings of mental illness among the those affected and those unaffected. It directly affects whether people in mental distress intend to seek help in the first place, and they have reported that it contributes to whether they feel able to disclose their problems. In essence, individuals with a mental illness expect to be discriminated against.
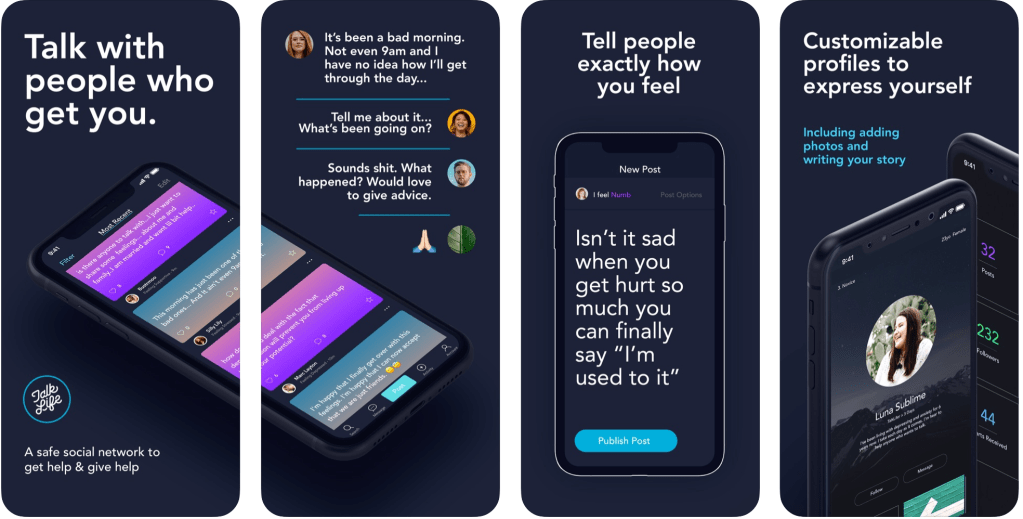
Where can I get help?
- Don’t be afraid to reach out. Contact the NAMI helpline to get you connected with resources.
- Seek out a mental health professional in order to get an accurate diagnosis. With this, you can begin to initiate a treatment plan.
- Remember that treatment is not “one-size-fits-all.” Some options include medication and/or counseling.
If you suspect someone is dealing with a mental illness, what can you do to help?
- Advocate for those who feel like they don’t have a voice. Everyone should have equal rights and opportunities, and having a mental illness doesn’t change that.
- Make the effort to learn more about mental health in order to help those affected in our community.